Cleft lip and cleft palate
| Cleft lip and palate | |
|---|---|
| Other names | Hare-lip, cleft lip and palate |
 | |
| Child with cleft lip and palate | |
| Specialty | Oral and Maxillofacial Surgery, Otorhinolaryngology, pediatrics |
| Symptoms | Opening in the upper lip that may extend into the nose or palate[1] |
| Complications | Feeding problems, speech problems, hearing problems, frequent ear infections[1] |
| Usual onset | Present at birth[1] |
| Causes | Usually unknown[1] |
| Risk factors | Smoking during pregnancy, diabetes, obesity, older mother, certain medications[1][2] |
| Treatment | Surgery, speech therapy, dental care[1] |
| Prognosis | Good (with treatment)[1] |
| Frequency | 1.5 per 1000 births (developed world)[2] |
| Deaths | 3,800 (2017)[3] |
A cleft lip contains an opening in the upper lip that may extend into the nose.[1] The opening may be on one side, both sides, or in the middle.[1] A cleft palate occurs when the palate (the roof of the mouth) contains an opening into the nose.[1] The term orofacial cleft refers to either condition or to both occurring together. These disorders can result in feeding problems, speech problems, hearing problems, and frequent ear infections.[1] Less than half the time the condition is associated with other disorders.[1]
Cleft lip and palate are the result of tissues of the face not joining properly during development.[1] As such, they are a type of birth defect.[1] The cause is unknown in most cases.[1] Risk factors include smoking during pregnancy, diabetes, obesity, an older mother, and certain medications (such as some used to treat seizures).[1][2] Cleft lip and cleft palate can often be diagnosed during pregnancy with an ultrasound exam.[1]
A cleft lip or palate can be successfully treated with surgery.[1] This is often done in the first few months of life for cleft lip and before eighteen months for cleft palate.[1] Speech therapy and dental care may also be needed.[1] With appropriate treatment, outcomes are good.[1]
Cleft lip and palate occurs in about 1 to 2 per 1000 births in the developed world.[2] Cleft lip is about twice as common in males as females, while cleft palate without cleft lip is more common in females.[2] In 2017, it resulted in about 3,800 deaths globally, down from 14,600 deaths in 1990.[3][4] Cleft lips are commonly known as hare-lips because of their resemblance to the lips of hares or rabbits.[5]
Signs and symptoms
Cleft lip
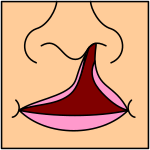
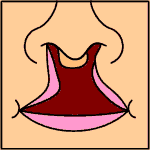
If the cleft does not affect the palate structure of the mouth, it is referred to as cleft lip. Cleft lip is formed in the top of the lip as either a small gap or an indentation in the lip (partial or incomplete cleft), or it continues into the nose (complete cleft). Lip cleft can occur as a one-sided (unilateral) or two-sided (bilateral) condition. It is due to the failure of fusion of the maxillary prominence and medial nasal processes (formation of the primary palate).
-
Unilateral incomplete
-
Unilateral complete
-
Bilateral complete
A mild form of a cleft lip is a microform cleft.[6] A microform cleft can appear as small as a little dent in the red part of the lip or look like a scar from the lip up to the nostril.[7] In some cases muscle tissue in the lip underneath the scar is affected and might require reconstructive surgery.[8] It is advised to have newborn infants with a microform cleft checked with a craniofacial team as soon as possible to determine the severity of the cleft.[9]
-
Six-month-old girl before going into surgery to have her unilateral complete cleft lip repaired
-
The same girl, one month after the surgery
-
The same girl, age eight, the scar almost gone
Cleft palate
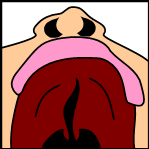
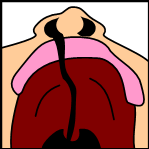
Cleft palate is a condition in which the two plates of the skull that form the hard palate (roof of the mouth) are not completely joined. The soft palate is in these cases cleft as well. In most cases, cleft lip is also present.
Palate cleft can occur as complete (soft and hard palate, possibly including a gap in the jaw) or incomplete (a 'hole' in the roof of the mouth, usually as a cleft soft palate). When cleft palate occurs, the uvula is usually split. It occurs due to the failure of fusion of the lateral palatine processes, the nasal septum, or the median palatine processes (formation of the secondary palate).
The hole in the roof of the mouth caused by a cleft connects the mouth directly to the inside of the nose.
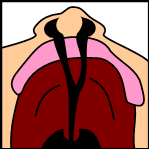
Note: the next images show the roof of the mouth. The top shows the nose, the lips are colored pink. For clarity the images depict a toothless infant.
-
Incomplete cleft palate
-
Unilateral complete lip and palate
-
Bilateral complete lip and palate
A result of an open connection between the mouth and inside the nose is called velopharyngeal insufficiency (VPI). Because of the gap, air leaks into the nasal cavity resulting in a hypernasal voice resonance and nasal emissions while talking.[10] Secondary effects of VPI include speech articulation errors (e.g., distortions, substitutions, and omissions) and compensatory misarticulations and mispronunciations (e.g., glottal stops and posterior nasal fricatives).[11] Possible treatment options include speech therapy, prosthetics, augmentation of the posterior pharyngeal wall, lengthening of the palate, and surgical procedures.[10]
Submucous cleft palate can also occur, which is a cleft of the soft palate with a split uvula, a furrow along the midline of the soft palate, and a notch in the back margin of the hard palate.[12] The diagnosis of submucous cleft palate often occurs late in children as a result of the nature of the cleft.[13] While the muscles of the soft palate are not joined, the mucosal membranes covering the roof of the mouth appear relatively normal and intact.[14]
Teeth
Tooth development can be delayed with increasing severity of CLP. Some of the dental problems affect the primary teeth, but most of the problems arise after the permanent teeth erupt. Problems may include fused teeth, missing teeth, and extra teeth erupting behind normal teeth. Missing teeth or extra teeth are both normal occurrences. Typically, the lateral incisors are missing. The enamel (outermost layer of the tooth) is commonly found to be hypomineralized and hypoplastic, making the teeth more likely to decay. As CLP can make oral hygiene more difficult, there is an increased rate of cavities.[15] In addition, abnormal positioning of individual teeth may affect occlusion, which can create an open bite or cross bite. This in turn can then affect the patient's speech.[16][17]
Complications

Cleft may cause problems with feeding, ear disease, speech, socialization, and cognition.
Due to lack of suction, an infant with a cleft may have trouble feeding. An infant with a cleft palate will have greater success feeding in a more upright position. Gravity will help prevent milk from coming through the baby's nose if he/she has cleft palate. Gravity feeding can be accomplished by using specialized equipment, such as the Haberman Feeder. Another equipment commonly used for gravity feeding is a customized bottle with a combination of nipples and bottle inserts. A large hole, crosscut, or slit in the nipple, a protruding nipple and rhythmically squeezing the bottle insert can result in controllable flow to the infant without the stigma caused by specialized equipment.
Individuals with cleft also face many middle ear infections which may eventually lead to hearing loss. The Eustachian tubes and external ear canals may be angled or tortuous, leading to food or other contamination of a part of the body that is normally self-cleaning. Hearing is related to learning to speak. Babies with palatal clefts may have compromised hearing and therefore, if the baby cannot hear, it cannot try to mimic the sounds of speech. Thus, even before expressive language acquisition, the baby with the cleft palate is at risk for receptive language acquisition. Because the lips and palate are both used in pronunciation, individuals with cleft usually need the aid of a speech therapist.
Tentative evidence has found that those with clefts perform less well at language.[18]
Psychosocial issues
There is research dedicated to the psychosocial development of individuals with cleft palate. A cleft palate/lip may impact an individual's self-esteem, social skills and behavior. Self-concept may be adversely affected by the presence of a cleft lip or cleft palate, particularly among girls.[19] Negative outcomes can also be associated with the long durations of hospitalization. Psychological issues could extend not just to the individual with CLP but also to their families, particularly their mothers, that experience varying levels of depression and anxiety.[20][21]
Research has shown that during the early preschool years (ages 3–5), children with cleft lip or cleft palate tend to have a self-concept that is similar to their peers without a cleft. However, as they grow older and their social interactions increase, children with clefts tend to report more dissatisfaction with peer relationships and higher levels of social anxiety. Experts conclude that this is probably due to the associated stigma of visible deformities and possible speech impediments. Children who are judged as attractive tend to be perceived as more intelligent, exhibit more positive social behaviors, and are treated more positively than children with cleft lip or cleft palate.[22] Children with clefts tend to report feelings of anger, sadness, fear, and alienation from their peers, but these children were similar to their peers in regard to "how well they liked themselves."
The relationship between parental attitudes and a child's self-concept is crucial during the preschool years. It has been reported that elevated stress levels in mothers correlated with reduced social skills in their children.[23] Strong parent support networks may help to prevent the development of negative self-concept in children with cleft palate.[24] In the later preschool and early elementary years, the development of social skills is no longer only impacted by parental attitudes but is beginning to be shaped by their peers. A cleft lip or cleft palate may affect the behavior of preschoolers. Experts suggest that parents discuss with their children ways to handle negative social situations related to their cleft lip or cleft palate. A child who is entering school should learn the proper (and age-appropriate) terms related to the cleft. The ability to confidently explain the condition to others may limit feelings of awkwardness and embarrassment and reduce negative social experiences.[25]
As children reach adolescence, the period of time between age 13 and 19, the dynamics of the parent-child relationship change as peer groups are now the focus of attention. An adolescent with cleft lip or cleft palate will deal with the typical challenges faced by most of their peers including issues related to self-esteem, dating and social acceptance.[26][27][28] Adolescents, however, view appearance as the most important characteristic, above intelligence and humor.[29] This being the case, adolescents are susceptible to additional problems because they cannot hide their facial differences from their peers. Adolescent boys typically deal with issues relating to withdrawal, attention, thought, and internalizing problems, and may possibly develop anxiousness-depression and aggressive behaviors.[28] Adolescent girls are more likely to develop problems relating to self-concept and appearance. Individuals with cleft lip or cleft palate often deal with threats to their quality of life for multiple reasons including unsuccessful social relationships, deviance in social appearance, and multiple surgeries.
Cause
Most clefts are polygenic and multifactorial in origin with many genetic and environmental factors contributing. Genetic factors cause clefts in 20% to 50% of the cases and the remaining clefts are attributable to either environmental factors (such as teratogens) or gene-environment interactions. The polygenic/multifactorial inheritance model predicts that most individuals will be born without clefts; however with a number of genetic or environmental factors, it can result in cleft formation.[17]
The development of the face is coordinated by complex morphogenetic events and rapid proliferative expansion, and is thus highly susceptible to environmental and genetic factors, rationalising the high incidence of facial malformations. During the first six to eight weeks of pregnancy, the shape of the embryo's head is formed. Five primitive tissue lobes grow:
- a) one from the top of the head down towards the future upper lip (frontonasal prominence);
- b-c) two from the cheeks, which meet the first lobe to form the upper lip (maxillar prominence);
- d-e) and just below, two additional lobes grow from each side, which form the chin and lower lip (mandibular prominence).
If these tissues fail to meet, a gap appears where the tissues should have joined (fused). This may happen in any single joining site, or simultaneously in several or all of them. The resulting birth defect reflects the locations and severity of individual fusion failures (e.g., from a small lip or palate fissure up to a completely malformed face).
The upper lip is formed earlier than the palate, from the first three lobes named a to c above. Formation of the palate is the last step in joining the five embryonic facial lobes, and involves the back portions of the lobes b and c. These back portions are called palatal shelves, which grow towards each other until they fuse in the middle.[30] This process is very vulnerable to multiple toxic substances, environmental pollutants, and nutritional imbalance. The biologic mechanisms of mutual recognition of the two cabinets, and the way they are glued together, are quite complex and obscure despite intensive scientific research.[30]
Orofacial clefts may be associated with a syndrome (syndromic) or may not be associated with a syndrome (nonsyndromic). Syndromic clefts are part of syndromes that are caused by a variety of factors such as environment and genetics or an unknown cause. Nonsyndromic clefts, which are not as common as syndromic clefts, also have a genetic cause.[31]
Genetics
Genetic factors contributing to cleft lip and cleft palate formation have been identified for some syndromic cases. Many clefts run in families, even though in some cases there does not seem to be an identifiable syndrome present.[32] A number of genes are involved including cleft lip and palate transmembrane protein 1 and GAD1,[33] One study found an association between mutations in the HYAL2 gene and cleft lip and cleft palate formation.[34]
Syndromes
- The Van der Woude syndrome is caused by a specific variation in the gene IRF6 that increases the occurrence of these deformities threefold.[35][36][37] Mutations in interferon regulatory factor 6 (IRF6) that cause cleft lip palate are also implicated in neural tube defects such as spina bifida.[38]
- Another syndrome, Siderius X-linked intellectual disability, is caused by mutations in the PHF8 gene (OMIM: 300263); in addition to cleft lip or palate, symptoms include facial dysmorphism and mild intellectual disability.[39]
In some cases, cleft palate is caused by syndromes that also cause other problems:
- Stickler syndrome can cause cleft lip and palate, joint pain, and myopia.[40][41]
- Loeys–Dietz syndrome can cause cleft palate or bifid uvula, hypertelorism, and aortic aneurysm.[42]
- Hardikar syndrome can cause cleft lip and palate, Hydronephrosis, Intestinal obstruction and other symptoms.[43]
- Cleft lip/palate may be present in many different chromosome disorders including Patau syndrome (trisomy 13).
- Malpuech facial clefting syndrome
- Hearing loss with craniofacial syndromes
- Popliteal pterygium syndrome
- Cornelia de Lange syndrome
- Treacher Collins syndrome
- Pierre Robin syndrome[44][31]
Specific genes
| Type | OMIM | Gene | Locus |
|---|---|---|---|
| OFC1 | 119530 | ? | 6p24 |
| OFC2 | 602966 | ? | 2p13 |
| OFC3 | 600757 | ? | 19q13 |
| OFC4 | 608371 | ? | 4q |
| OFC5 | 608874 | MSX1 | 4p16.1 |
| OFC6 | 608864 | ? | 1q |
| OFC7 | 600644) | PVRL1 | 11q |
| OFC8 | 129400 | TP63 | 3q27 |
| OFC9 | 610361 | ? | 13q33.1-q34 |
| OFC10 | 601912 | SUMO1 | 2q32.2-q33 |
| OFC11 | 600625 | BMP4 | 14q22 |
| OFC12 | 612858 | ? | 8q24.3 |
Many genes associated with syndromic cases of cleft lip/palate (see above) have been identified to contribute to the incidence of isolated cases of cleft lip/palate. This includes in particular sequence variants in the genes IRF6, PVRL1 and MSX1.[45] The understanding of the genetic complexities involved in the morphogenesis of the midface, including molecular and cellular processes, has been greatly aided by research on animal models, including of the genes BMP4, SHH, SHOX2, FGF10 and MSX1.[45]
Environmental factors
Environmental influences may also cause, or interact with genetics to produce, orofacial clefts. An example of the link between environmental factors and genetics comes from a research on mutations in the gene PHF8. The research found that PHF8 encodes for a histone lysine demethylase,[46] and is involved in epigenetic regulation. The catalytic activity of PHF8 depends on molecular oxygen,[46] a factor considered important from reports on increased incidence of cleft lip/palate in mice that have been exposed to hypoxia early during pregnancy.[47]
Cleft lip and other congenital abnormalities have also been linked to maternal hypoxia caused by maternal smoking,[48] with the estimated attributable fraction of orofacial clefts due to smoking in early pregnancy being 6.1%. Orofacial clefts occur very early in pregnancy and so smoking cessation right after recognition of pregnancy is unlikely to reduce the exposure during the critical time period.[49]
Maternal alcohol use has also been linked to cleft lip and palate due to the effects on the cranial neural crest cells. The degree of the effect, however, is unknown and requires further research.[50] Some forms of maternal hypertension treatment have been linked to cleft lip and palate.[51] Other environmental factors that have been studied include seasonal causes (such as pesticide exposure); maternal diet and vitamin intake; retinoids (members of the vitamin A family); anticonvulsant drugs; nitrate compounds; organic solvents; parental exposure to lead; alcohol; cigarette use; and a number of other psychoactive drugs (e.g. cocaine, crack cocaine, heroin).
Current research continues to investigate the extent to which folic acid can reduce the incidence of clefting.[52] Folic acid alone or in combination with vitamins and minerals prevents neural tube defects but does not have a clear effect on cleft lip palate incidence.[53] The mechanism behind beneficial folate supplementation is due to folate playing a pivotal role in DNA synthesis and methylation and contributes to both development and gene expression.[54]
Diagnosis
Traditionally, the diagnosis is made at the time of birth by physical examination. Recent advances in prenatal diagnosis have allowed obstetricians to diagnose facial clefts in utero with ultrasonography.[55]
Clefts can also affect other parts of the face, such as the eyes, ears, nose, cheeks, and forehead. In 1976, Paul Tessier described fifteen lines of cleft. Most of these craniofacial clefts are even rarer and are frequently described as Tessier clefts using the numerical locator devised by Tessier.[56]
Classification
Cleft lip and cleft palate is an "umbrella term" for a collection of orofacial clefts. It includes clefting of the upper lip, the maxillary alveolus (dental arch), and the hard or soft palate, in various combinations. Proposed anatomic combinations include:[57]
- cleft lip
- cleft lip and alveolus
- cleft lip, alveolus, and palate
- cleft lip and palate (with an intact alveolus)
- cleft palate
Prenatal diagnosis
Cleft lip with or without palate is classified as the most common congenital birth defect. It has been noted that the prevalence of orofacial clefts varies by race. The highest number of cases have been recorded among Asians and Native Americans, followed by Europeans, Hispanics and African-Americans. The critical period for cleft development ranges from the 4th to the 12th week of intrauterine life. Clefts of the primary palate develop between the 4th and 7th weeks of intrauterine life, while clefts of the secondary palate develop between the 8th and 12th embryonic weeks.
Accurate evaluation of craniofacial malformations is usually possible with the ultrasound scan performed during pregnancy. This is however not a routine procedure according to the American Institute of Ultrasound in Medicine. The accuracy of ultrasonography for prenatal diagnosis of cleft lip +/- palate is dependent on the experience of the sonologist, maternal body type, foetal position, the amount of amniotic fluid and the type of cleft.
Prenatal diagnosis enables appropriate and timely education and discussion with parents by the cleft team. This helps improve the quality of treatment received by the child and improves quality of life.
An accurate prenatal diagnosis of the CLP anomaly is critical for establishing long-term treatment planning, prediction of treatment outcome, and discussion and education of the parent. Although there is no intrauterine treatment for CLP, both mother and child benefit from early diagnosis and education. A multidisciplinary team approach is now accepted as the standard of care in dealing with CLP patients.
The time period immediately after the diagnosis and the first year after the birth is most challenging for parents. A systematically planned treatment plan and support system will help assist parents. The ultimate aim is to help educate parents and create awareness so as to improve care provided for the child.[58]
Treatment
Cleft lip and palate is very treatable; however, the kind of treatment depends on the type and severity of the cleft.
Most children with a form of clefting are monitored by a cleft palate team or craniofacial team through young adulthood.[59] Care can be lifelong and are looked after by craniofacial cleft teams often consist of: cleft surgeons, orthodontists, speech and language therapists, restorative dentists, psychologists, ENT surgeons and audio-logical physicians.[60]: 255 Treatment procedures can vary between craniofacial teams. For example, some teams wait on jaw correction until the child is aged 10 to 12 (argument: growth is less influential as deciduous teeth are replaced by permanent teeth, thus saving the child from repeated corrective surgeries), while other teams correct the jaw earlier (argument: less speech therapy is needed than at a later age when speech therapy becomes harder). Within teams, treatment can differ between individual cases depending on the type and severity of the cleft.
Cleft lip
Within the first 2–3 months after birth, surgery is performed to close the cleft lip. While surgery to repair a cleft lip can be performed soon after birth, often the preferred age is at approximately 10 weeks of age, following the "rule of 10s" coined by surgeons Wilhelmmesen and Musgrave in 1969 (the child is at least 10 weeks of age; weighs at least 10 pounds, and has at least 10g/dL hemoglobin).[61][62] If the cleft is bilateral and extensive, two surgeries may be required to close the cleft, one side first, and the second side a few weeks later. The most common procedure to repair a cleft lip is the Millard procedure pioneered by Ralph Millard. Millard performed the first procedure at a Mobile Army Surgical Hospital (MASH) unit in Korea.[63]
Often an incomplete cleft lip requires the same surgery as complete cleft. This is done for two reasons. Firstly the group of muscles required to purse the lips run through the upper lip. To restore the complete group a full incision must be made. Secondly, to create a less obvious scar the surgeon tries to line up the scar with the natural lines in the upper lip (such as the edges of the philtrum) and tuck away stitches as far up the nose as possible. Incomplete cleft gives the surgeon more tissue to work with, creating a more supple and natural-looking upper lip.
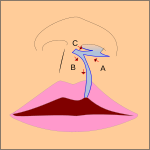
-
The blue lines indicate incisions.
-
Movement of the flaps; flap A is moved between B and C. C is rotated slightly while B is pushed down.
-
Pre-operation
-
Post-operation, the lip is swollen from surgery and will look more natural within weeks. See photos in the section above.
Pre-surgical devices
In some cases of a severe bilateral complete cleft, the premaxillary segment will be protruded far outside the mouth.
Nasoalveolar molding prior to surgery can improve long-term nasal symmetry where there is complete unilateral cleft lip–cleft palate, compared to correction by surgery alone, according to a retrospective cohort study.[64] In this study, significant improvements in nasal symmetry were observed in multiple areas including measurements of the projected length of the nasal ala (lateral surface of the external nose), position of the superoinferior alar groove, position of the mediolateral nasal dome, and nasal bridge deviation. "The nasal ala projection length demonstrated an average ratio of 93.0 percent in the surgery-alone group and 96.5 percent in the nasoalveolar molding group," this study concluded. A systematic review found in conclusion that nasoalveolar molding had a positive effect on the primary surgery of cleft lip/or palate treatment and aesthetics.[65]
Cleft palate

Often a cleft palate is temporarily covered by a palatal obturator (a prosthetic device made to fit the roof of the mouth covering the gap). This device re-positions displaced alveolar segments and helps reduce the cleft lip separation. The obturator will improve speech as there's now proper airflow and improve feeding and breathing as the gap in the hard and soft palate is closed over so cannot affect it.[60]: 257
Cleft palate can also be corrected by surgery, usually performed between 6 and 12 months. Approximately 20–25% only require one palatal surgery to achieve a competent velopharyngeal valve capable of producing normal, non-hypernasal speech. However, combinations of surgical methods and repeated surgeries are often necessary as the child grows. One of the new innovations of cleft lip and cleft palate repair is the Latham appliance.[66] The Latham is surgically inserted by use of pins during the child's fourth or fifth month. After it is in place, the doctor, or parents, turn a screw daily to bring the cleft together to assist with future lip or palate repair.
If the cleft extends into the maxillary alveolar ridge, the gap is usually corrected by filling the gap with bone tissue. The bone tissue can be acquired from the individual's own chin, rib or hip.
At age 1–7 years the child is regularly reviewed by the cleft team.[60]: 257
Age 7–12 years, for the children born with alveolar clefts, they may need to have a secondary alveolar bone graft. This is where autogenous cancellous bone from a donor site (often the pelvic bone) is transplanted into the alveolar cleft region. This transplant of bone will close the osseous cleft of the alveolus, close any oro-nasal fistulae and will become integrated with the maxillary bone. It provides bone for teeth to erupt into and to allow implants to be placed as a possible future treatment option. The procedure should be carried out before the upper canine has erupted. Ideally the root of the canine should be one to two-thirds formed and that there is a space available to place the bone graft. Radio-graphs are taken to determine the quantity of missing bone in the cleft area.[60]: 258
Other surgeries
Orthognathic surgery – surgical cutting of bone to realign the upper jaw (osteotomy). The bone is cut then re-positioned and held together by wires or rigid fixation plates to ensure there's no anterior-posterior discrepancy, also to reduce scarring as it reduces growth. Single piece or multi-piece osteotomy exist. Single piece osteotomy is carried out where there is sufficient alveolar continuity achieved from a successful bone graft. Multi piece osteotomy is performed when there is a notable residual alveolar defect with a dental gap and oronasal fistula (communication between the oral and nasal cavities). The goal of both single and multi piece osteotomy is to displace the maxilla forward to obtain adequate occlusion as well to provide better support for upper lip and the nose and to close any fistulae.[67]
Distraction osteogenesis – bone lengthening by gradual distraction. This involves cutting bone and moving ends apart incrementally to allow new bone to form in the gap. This consists of several phases. After attachment of the distracting device and the bone cuts, there is a latency phase of 3–7 days when a callus forms. In the activation phase distraction of the callus induces bony ingrowth which can last up to 15 days depending on the required distraction. Once the required bone length is reached, the distraction device is left to remain in situ as it acts as a rigid skeletal fixation device until the new bone has matured (known as the consolidation period).[67]
Speech
Velopharyngeal insufficiency (VPI) can occur as a result of an unrepaired or repaired cleft lip and palate. VPI is the inability of the soft palate to close tightly against the back of the throat during speech, resulting in incomplete velopharyngeal closure. In turn, this results in speech abnormalities. Velopharyngeal closure is necessary during speech because it forms a seal between the nose and mouth, allowing the production of normal speech sounds. VPI can cause hypernasality (excessive nasal resonance), hyponasality (reduced nasal resonance), or a mixed nasal resonance, which is when hypernasality and hyponasality occur simultaneously.[68] In addition, CLP may cause abnormal positioning of individual teeth, which can in turn affect the patient's ability to make certain sounds when speaking such as the "f" or "v" sound and can also result in a lisp. The changes in speech may also be a manifestation on CLP's effects on the patient's occlusion.[16][17]
Hearing
Children with cleft palate have a very high risk of developing a middle ear infection, specifically otitis media. This is due to the immature development of the different bones and muscles in the ear. Otitis media is caused by the obstruction of the Eustachian tube, negative middle ear pressure and fluid build-up in the normally air-filled space of the middle ear.[69] This is associated with hearing impairment or loss. The insertion of a ventilation tube into the eardrum is a surgical treatment option commonly used to improve hearing in children with otitis media.[70] In addition, breast milk has been proven to decrease the incidence of otitis media in infants with clefts.[16]
Feeding
There are different options on how to feed a baby with cleft lip or cleft palate which include: breast-feeding, bottle feeding, spoon feeding and syringe feeding. Although breast-feeding is challenging, it improves weight-gain compared to spoon-feeding.[71] Nasal regurgitation is common due to the open space between the oral cavity and the nasal cavity. Bottle feeding can help (with squeezable bottles being easier to use than rigid bottles). In addition, maxillary plates can be added to aid in feeding. Whatever feeding method is established, it is important to keep the baby's weight gain and hydration monitored. Infants with cleft lip or palate may require supplemental feeds for adequate growth and nutrition. Breast feeding position as suggested by specialists can also improve success rate.[72]
Breast-feeding
Babies with cleft lip are more likely to breastfeed successfully than those with cleft palate and cleft lip and palate. Larger clefts of the soft or hard palate may not be able to generate suction as the oral cavity cannot be separated from the nasal cavity when feeding which leads to fatigue, prolonged feeding time, impaired growth and nutrition. Changes in swallowing mechanics may result in coughing, choking, gagging and nasal regurgitation. Even after cleft repair, the problem may still persist as significant motor learning of swallowing and sucking was absent for many months before repair.[73] These difficulties in feeding may result in secondary problems such as poor weight gain, excessive energy expenditure during feeding, lengthy feeding times, discomfort during feeding, and stressful feeding interactions between the infant and the mother. A potential source of discomfort for the baby during or after feeding is bloating or frequent "spit up" which is due to the excessive air intake through the nose and mouth in the open cleft.[16] Babies with cleft lip and or palate should be evaluated individually taking into account the size and location of the cleft and the mother's previous experience with breastfeeding.[71]
Another option is feeding breast milk via bottle or syringe. Since babies with clip lip and cleft palate generate less section when breastfeeding, their nutrition, hydration and weight gain may be affected. This may result in the need for supplemental feeds. Modifying the position of holding the baby may increase the effectiveness and efficiency of breastfeeding.
Alternative Feeding Methods
Preoperative feeding – using a squeezable bottle instead of a rigid bottle can allow a higher volume of food intake and less effort to extract food. Using a syringe is practical, easy to perform and allows greater administered volume of food. It also means there will be weight gain and less time spent feeding.[74]
Post-operative feeding (isolated lip repair, or lip repair associated or not with palatoplasty) – post palatoplasty, some studies believe that inappropriate negative pressure on the suture line may affect results. Babies can be fed by a nasogastric tube instead. Studies suggest babies required less analgesics and shorter hospital stay with nasogastric feeding post-surgery. With bottle-feeding, there was higher feeding rejection and pain and required more frequent and prolonged feeding times.[74]
Treatment schedule
Each person's treatment schedule is individualized. The table below shows a common sample treatment schedule. The colored squares indicate the average timeframe in which the indicated procedure occurs. In some cases, this is usually one procedure, for example lip repair. In other cases, it is an ongoing therapy, for example speech therapy. In most cases of cleft lip and palate that involve the alveolar bone, patients will need a treatment plan including the prevention of cavities, orthodontics, alveolar bone grafting, and possibly jaw surgery.[75]
| Age | 0m
|
3m
|
6m
|
9m
|
1y
|
2y
|
3y
|
4y
|
5y
|
6y
|
7y
|
8y
|
9y
|
10y
|
11y
|
12y
|
13y
|
14y
|
15y
|
16y
|
17y
|
18y
|
| Palatal obturator | ||||||||||||||||||||||
| Repair cleft lip | ||||||||||||||||||||||
| Repair soft palate | ||||||||||||||||||||||
| Repair hard palate | ||||||||||||||||||||||
| Tympanostomy tube | ||||||||||||||||||||||
| Speech therapy/pharyngoplasty | ||||||||||||||||||||||
| Alveolar cleft grafting | ||||||||||||||||||||||
| Orthodontics | ||||||||||||||||||||||
| Orthognathic surgery |
Cleft team
People with CLP present with a multiplicity of problems. Therefore, effective management of CLP involves a wide range of specialists. The current model for delivery of this care is the multidisciplinary cleft team. This is a group of individuals from different specialist backgrounds who work closely together to provide patients with comprehensive care from birth through adolescence. This system of delivery of care enables the individuals within the team to function in an interdisciplinary way, so that all aspects of care for CLP patients can be provided in the best way possible.[76]
Outcomes assessment
Measuring the outcomes of CLP treatment has been laden with difficulty due to the complexity and longitudinal nature of cleft care, which spans birth through young adulthood. Prior attempts to study the effectiveness of specific interventions or overall treatment protocols have been hindered by a lack of data standards for outcomes assessment in cleft care.[citation needed]
The International Consortium for Health Outcome Measurement (ICHOM) has proposed the Standard Set of Outcome Measures for Cleft Lip and Palate.[77][78] The ICHOM Standard Set includes measures for many of the important outcome domains in cleft care (hearing, breathing, eating/drinking, speech, oral health, appearance and psychosocial well-being). It includes clinician-reported, patient-reported, and family-reported outcome measures.
Epidemiology
Cleft lip and palate occurs in about 1 to 2 per 1000 births in the developed world.[2]
Rates for cleft lip with or without cleft palate and cleft palate alone varies within different ethnic groups.
According to CDC, the prevalence of cleft palate in the United States is 6.35/10000 births and the prevalence of cleft lip with or without cleft palate is 10.63/10000 births.[79] The highest prevalence rates for cleft lip, either with or without cleft palate are reported for Native Americans and Asians. Africans have the lowest prevalence rates.[80]
- Native Americans: 3.74/1000
- Japanese: 0.82/1000 to 3.36/1000
- Chinese: 1.45/1000 to 4.04/1000
- White Americans: 1.43/1000 to 1.86/1000
- Latin Americans: 1.04/1000
- Africans: 0.18/1000 to 1.67/1000
Cleft lip and cleft palate caused about 3,800 deaths globally in 2017, down from 14,600 deaths in 1990.[4]
Prevalence of "cleft uvula" has varied from 0.02% to 18.8% with the highest numbers found among Chippewa and Navajo and the lowest generally in Africans.[81][82]
Society and culture

Handicap law and abortion controversies
In some countries, cleft lip or palate deformities are considered reasons (either generally tolerated or officially sanctioned) to perform an abortion beyond the legal fetal age limit, even though the fetus is not in jeopardy of life or limb.[83][84] Some political opponents contend this practice amounts to eugenics based on cosmetic defects rather than practical definitions of a disability.[85]
Works of fiction
The eponymous hero of J. M. Coetzee's 1983 novel Life & Times of Michael K has a cleft lip that is never corrected. In the 1920 novel Growth of the Soil, by Norwegian writer Knut Hamsun, Inger (wife of the main character) has an uncorrected cleft lip which puts heavy limitations on her life, even causing her to kill her own child, who is also born with a cleft lip. The protagonist of the 1924 novel Precious Bane, by English writer Mary Webb, is a young woman living in 19th-century rural Shropshire who eventually comes to feel that her deformity is the source of her spiritual strength. The book was later adapted for television by both the BBC and ORTF in France. Similarly, the main character in Graham Greene's 1936 crime noir novel A Gun for Sale, Raven, has a cleft lip which he is sensitive about, and is described as "an ugly man dedicated to ugly deeds". In the 1976 Patricia A. McKillip novel The Night Gift, one of the high-school aged protagonists is shy because she has a cleft lip, but learns to have more confidence in herself.
In the first edition of Harry Potter and the Chamber of Secrets, one of the people Gilderoy Lockhart stole credit from was a witch with a harelip who banished the Bandon Banshee. In later editions, this was changed to a witch with a hairy chin.[86]
In chapter 26 of Mark Twain's The Adventures of Huckleberry Finn, Huck Finn meets the three Wilks sisters, Mary Jane, Susan, and Joanna. Joanna is described as, "the one who gives herself to good works and has a hare-lip." As a form of offensive synecdoche, Huck Finn refers to Joanna as "the hare-lip" rather than by her name.
Cleft lip and cleft palate are often portrayed negatively in popular culture. Examples include Oddjob, the secondary villain of the James Bond novel Goldfinger by Ian Fleming (the film adaptation does not mention this but leaves it implied) and serial killer Francis Dolarhyde in the novel Red Dragon and its screen adaptations, Manhunter, Red Dragon, and Hannibal.[87] The portrayal of enemy characters with cleft lips and cleft palates, dubbed mutants, in the 2019 video game Rage 2 left Chris Plante of Polygon wondering if the condition would ever be portrayed positively.[88][89]
Notable cases
| Name | Comments | |
|---|---|---|
| Jerry Byrd | American sportswriter for the Shreveport Journal, 1957–1991, and Bossier Press-Tribune, 1993–2012; born with cleft lip and without cleft palate | [90] |
| John Henry "Doc" Holliday | American dentist, gambler and gunfighter of the American Old West, who is usually remembered for his friendship with Wyatt Earp and the Gunfight at the O.K. Corral | [91] |
| Tutankhamen | Egyptian pharaoh who may have had a slightly cleft palate according to diagnostic imaging | [92] |
| Thorgils Skarthi | Thorgils 'the hare-lipped'—a 10th-century Viking warrior and founder of Scarborough, England. | [93] |
| Tad Lincoln | Fourth and youngest son of President Abraham Lincoln | [94] |
| Carmit Bachar | American dancer and singer | [95][96] |
| Jürgen Habermas | German philosopher and sociologist | [97] |
| Ljubo Milicevic | Australian professional footballer | [98] |
| Stacy Keach | American actor and narrator | [99] |
| Cheech Marin | American actor and comedian | [100] |
| Owen Schmitt | American football fullback | [101] |
| Tim Lott | English author and journalist | [102] |
| Richard Hawley | English musician | [102] |
| Dario Šarić | Croatian professional basketball player | [103] |
| Antoinette Bourignon | Flemish mystic | [104] |
| Tom Burke | English actor | [105] |
| Franz Rogowski | German actor | [106] |
Other animals
Cleft lips and palates are occasionally seen in cattle and dogs, and rarely in goats, sheep, cats, horses, pandas and ferrets. Most commonly, the defect involves the lip, rhinarium, and premaxilla. Clefts of the hard and soft palate are sometimes seen with a cleft lip. The cause is usually hereditary. Brachycephalic dogs such as Boxers and Boston Terriers are most commonly affected.[107] An inherited disorder with incomplete penetrance has also been suggested in Shih tzus, Swiss Sheepdogs, Bulldogs, and Pointers.[108] In horses, it is a rare condition usually involving the caudal soft palate.[109] In Charolais cattle, clefts are seen in combination with arthrogryposis, which is inherited as an autosomal recessive trait. It is also inherited as an autosomal recessive trait in Texel sheep. Other contributing factors may include maternal nutritional deficiencies, exposure in utero to viral infections, trauma, drugs, or chemicals, or ingestion of toxins by the mother, such as certain lupines by cattle during the second or third month of gestation.[110] The use of corticosteroids during pregnancy in dogs and the ingestion of Veratrum californicum by pregnant sheep have also been associated with cleft formation.[111]
Difficulty with nursing is the most common problem associated with clefts, but aspiration pneumonia, regurgitation, and malnutrition are often seen with cleft palate and is a common cause of death. Providing nutrition through a feeding tube is often necessary, but corrective surgery in dogs can be done by the age of twelve weeks.[107] For cleft palate, there is a high rate of surgical failure resulting in repeated surgeries.[112] Surgical techniques for cleft palate in dogs include prosthesis, mucosal flaps, and microvascular free flaps.[113] Affected animals should[opinion] not be bred due to the hereditary nature of this condition.[citation needed]
-
Cleft lip in a Boxer
-
Cleft lip in a Boxer with premaxillary involvement
-
Same dog as picture on left, one year later
See also
- Smile Pinki
- Palatal obturator
- Vomer flap surgery
- Cleft lip and palate organisations
- Face and neck development of the embryo
References
- ^ a b c d e f g h i j k l m n o p q r s t u "Facts about Cleft Lip and Cleft Palate". October 20, 2014. Archived from the original on May 8, 2015. Retrieved May 8, 2015.
- ^ a b c d e f Watkins SE, Meyer RE, Strauss RP, Aylsworth AS (April 2014). "Classification, epidemiology, and genetics of orofacial clefts". Clinics in Plastic Surgery. 41 (2): 149–163. doi:10.1016/j.cps.2013.12.003. PMID 24607185.
- ^ a b "Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017". Lancet. 392 (10159): 1736–1788. November 2018. doi:10.1016/S0140-6736(18)32203-7. PMC 6227606. PMID 30496103.
- ^ a b "GBD Results Tool | GHDx". ghdx.healthdata.org. Retrieved August 2, 2019.
- ^ Boklage CE (2010). How new humans are made cells and embryos, twins and chimeras, left and right, mind/selfsoul, sex, and schizophrenia. Singapore: World Scientific. p. 283. ISBN 978-981-283-514-7. Archived from the original on September 10, 2017.
- ^ Kim EK, Khang SK, Lee TJ, Kim TG (May 2010). "Clinical features of the microform cleft lip and the ultrastructural characteristics of the orbicularis oris muscle". The Cleft Palate-Craniofacial Journal. 47 (3): 297–302. doi:10.1597/08-270.1. PMID 19860522. S2CID 71448247.[permanent dead link]
- ^ Yuzuriha S, Mulliken JB (November 2008). "Minor-form, microform, and mini-microform cleft lip: anatomical features, operative techniques, and revisions". Plastic and Reconstructive Surgery. 122 (5): 1485–1493. doi:10.1097/PRS.0b013e31818820bc. PMID 18971733. S2CID 8551875.
- ^ Tosun Z, Hoşnuter M, Sentürk S, Savaci N (2003). "Reconstruction of microform cleft lip". Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 37 (4): 232–235. doi:10.1080/02844310310016412. PMID 14582757. S2CID 40850672.
- ^ Tollefson TT, Humphrey CD, Larrabee WF, Adelson RT, Karimi K, Kriet JD (2011). "The spectrum of isolated congenital nasal deformities resembling the cleft lip nasal morphology". Archives of Facial Plastic Surgery. 13 (3): 152–160. doi:10.1001/archfacial.2011.26. PMID 21576661.
- ^ a b Sloan GM (March 2000). "Posterior pharyngeal flap and sphincter pharyngoplasty: the state of the art". The Cleft Palate-Craniofacial Journal. 37 (2): 112–122. doi:10.1597/1545-1569(2000)037<0112:PPFASP>2.3.CO;2. PMID 10749049.
- ^ Hill JS (2001). "Velopharyngeal insufficiency: An update on diagnostic and surgical techniques". Current Opinion in Otolaryngology & Head and Neck Surgery. 9 (6): 365–8. doi:10.1097/00020840-200112000-00005. S2CID 76256148.
- ^ Kaplan EN (October 1975). "The occult submucous cleft palate". The Cleft Palate Journal. 12: 356–368. PMID 1058746.
- ^ Hanny KH, de Vries IA, Haverkamp SJ, Oomen KP, Penris WM, Eijkemans MJ, et al. (January 2016). "Late detection of cleft palate". European Journal of Pediatrics. 175 (1): 71–80. doi:10.1007/s00431-015-2590-9. PMC 4709386. PMID 26231683.
- ^ "Cleft Lip and Palate". American-Speech-Language-Hearing Association. Retrieved May 9, 2019.
- ^ "Index", Orthodontics: Principles and Practice, John Wiley & Sons, Ltd,., August 23, 2013, pp. 355–370, doi:10.1002/9781118785041.index, ISBN 978-1-118-78504-1
- ^ a b c d Goel S (2015). Feeding in Cleft Lip And Cleft Palata Infants. Saarbrücken, Germany: LAP LAMBERT Academic Publishing. pp. 20–22. ISBN 978-3-659-38212-3.
- ^ a b c Peterson-Falzone SJ, Trost-Cardamone JE, Karnell MP, Hardin-Jones MA (September 21, 2016). The clinician's guide to treating cleft palate speech (Second ed.). St. Louis, Missouri: Elsevier. ISBN 978-0-323-33934-6. OCLC 936145822.
- ^ Roberts RM, Mathias JL, Wheaton P (August 2012). "Cognitive functioning in children and adults with nonsyndromal cleft lip and/or palate: a meta-analysis". Journal of Pediatric Psychology. 37 (7): 786–797. doi:10.1093/jpepsy/jss052. PMID 22451260.
- ^ Leonard BJ, Brust JD, Abrahams G, Sielaff B (October 1991). "Self-concept of children and adolescents with cleft lip and/or palate". The Cleft Palate-Craniofacial Journal. 28 (4): 347–353. doi:10.1597/1545-1569(1991)028<0347:SCOCAA>2.3.CO;2. PMID 1742302.
- ^ Al-Namankany A, Alhubaishi A (August 2018). "Effects of cleft lip and palate on children's psychological health: A systematic review". Journal of Taibah University Medical Sciences. 13 (4): 311–318. doi:10.1016/j.jtumed.2018.04.007. PMC 6694901. PMID 31435341.
- ^ Hunt O, Burden D, Hepper P, Johnston C (June 2005). "The psychosocial effects of cleft lip and palate: a systematic review". European Journal of Orthodontics. 27 (3): 274–285. doi:10.1093/ejo/cji004. PMID 15947228.
- ^ Tobiasen JM (July 1984). "Psychosocial correlates of congenital facial clefts: a conceptualization and model". The Cleft Palate Journal. 21 (3): 131–139. PMID 6592056.
- ^ Pope AW, Ward J (September 1997). "Self-perceived facial appearance and psychosocial adjustment in preadolescents with craniofacial anomalies". The Cleft Palate-Craniofacial Journal. 34 (5): 396–401. doi:10.1597/1545-1569(1997)034<0396:SPFAAP>2.3.CO;2. PMID 9345606.
- ^ Bristow & Bristow 2007, pp. 82–92
- ^ "Cleft Palate Foundation". Archived from the original on July 1, 2007. Retrieved July 1, 2007.
- ^ Snyder HT, Bilboul MJ, Pope AW (September 2005). "Psychosocial adjustment in adolescents with craniofacial anomalies: a comparison of parent and self-reports". The Cleft Palate-Craniofacial Journal. 42 (5): 548–555. CiteSeerX 10.1.1.624.1274. doi:10.1597/04-078R.1. PMID 16149838. S2CID 37357550.
- ^ Endriga MC, Kapp-Simon KA (January 1999). "Psychological issues in craniofacial care: state of the art". The Cleft Palate-Craniofacial Journal. 36 (1): 3–11. doi:10.1597/1545-1569(1999)036<0001:PIICCS>2.3.CO;2. PMID 10067755.
- ^ a b Pope AW, Snyder HT (July 2005). "Psychosocial adjustment in children and adolescents with a craniofacial anomaly: age and sex patterns". The Cleft Palate-Craniofacial Journal. 42 (4): 349–354. doi:10.1597/04-043R.1. PMID 16001914. S2CID 31313562.
- ^ Prokhorov AV, Perry CL, Kelder SH, Klepp KI (1993). "Lifestyle values of adolescents: results from Minnesota Heart Health Youth Program". Adolescence. 28 (111): 637–647. PMID 8237549.
- ^ a b Dudas M, Li WY, Kim J, Yang A, Kaartinen V (2007). "Palatal fusion - where do the midline cells go? A review on cleft palate, a major human birth defect". Acta Histochemica. 109 (1): 1–14. doi:10.1016/j.acthis.2006.05.009. PMID 16962647.
- ^ a b Meeks NJ, Saenz M, Tsai AC, Elias ER (2018). "Genetics & Dysmorphology". In Hay WW, Levin MJ, Deterding RR, Abzug MJ (eds.). Current Diagnosis & Treatment: Pediatrics (24th ed.). McGraw-Hill Education. Retrieved August 6, 2019.
- ^ Beaty TH, Ruczinski I, Murray JC, Marazita ML, Munger RG, Hetmanski JB, et al. (September 2011). "Evidence for gene-environment interaction in a genome wide study of nonsyndromic cleft palate". Genetic Epidemiology. 35 (6): 469–478. doi:10.1002/gepi.20595. PMC 3180858. PMID 21618603.
- ^ Kanno K, Suzuki Y, Yamada A, Aoki Y, Kure S, Matsubara Y (May 2004). "Association between nonsyndromic cleft lip with or without cleft palate and the glutamic acid decarboxylase 67 gene in the Japanese population". American Journal of Medical Genetics. Part A. 127A (1): 11–16. doi:10.1002/ajmg.a.20649. PMID 15103710. S2CID 30016360.
- ^ Sandoiu A (January 17, 2017). "Scientists find genetic mutation that causes cleft lip and palate, heart defects". Medical News Today. Archived from the original on January 29, 2017. Retrieved January 31, 2017.
- ^ Dixon MJ, Marazita ML, Beaty TH, Murray JC (March 2011). "Cleft lip and palate: understanding genetic and environmental influences". Nature Reviews. Genetics. 12 (3): 167–178. doi:10.1038/nrg2933. PMC 3086810. PMID 21331089.
- ^ Zucchero TM, Cooper ME, Maher BS, Daack-Hirsch S, Nepomuceno B, Ribeiro L, et al. (August 2004). "Interferon regulatory factor 6 (IRF6) gene variants and the risk of isolated cleft lip or palate". The New England Journal of Medicine. 351 (8): 769–780. doi:10.1056/NEJMoa032909. PMID 15317890. S2CID 3324418.
- ^ "Cleft palate genetic clue found". BBC News. August 30, 2004. Archived from the original on February 8, 2007. Retrieved July 1, 2007.
- ^ Kousa YA, Zhu H, Fakhouri WD, Lei Y, Kinoshita A, Roushangar RR, et al. (May 2019). "The TFAP2A-IRF6-GRHL3 genetic pathway is conserved in neurulation". Human Molecular Genetics. 28 (10): 1726–1737. doi:10.1093/hmg/ddz010. PMC 6494790. PMID 30689861.
- ^ Siderius LE, Hamel BC, van Bokhoven H, de Jager F, van den Helm B, Kremer H, et al. (July 1999). "X-linked mental retardation associated with cleft lip/palate maps to Xp11.3-q21.3". American Journal of Medical Genetics. 85 (3): 216–220. doi:10.1002/(SICI)1096-8628(19990730)85:3<216::AID-AJMG6>3.0.CO;2-X. PMID 10398231.
- ^ Kronwith SD, Quinn G, McDonald DM, Cardonick E, Onyx P, LaRossa D, et al. (1990). "Stickler's syndrome in the Cleft Palate Clinic". Journal of Pediatric Ophthalmology and Strabismus. 27 (5): 265–267. doi:10.3928/0191-3913-19900901-12. PMID 2246742.
- ^ Mrugacz M, Sredzińska-Kita D, Bakunowicz-Lazarczyk A, Piszcz M (2005). "[High myopia as a pathognomonic sign in Stickler's syndrome]". Klinika Oczna (in Polish). 107 (4–6): 369–371. PMID 16118961.
- ^ Sousa SB, Lambot-Juhan K, Rio M, Baujat G, Topouchian V, Hanna N, et al. (May 2011). "Expanding the skeletal phenotype of Loeys-Dietz syndrome". American Journal of Medical Genetics. Part A. 155A (5): 1178–1183. doi:10.1002/ajmg.a.33813. PMID 21484991. S2CID 27999412.
- ^ Hardikar syndrome symptoms
- ^ Wall J, Albanese CT (2015), Doherty GM (ed.), "Pediatric Surgery", CURRENT Diagnosis & Treatment: Surgery (14th ed.), McGraw-Hill Education, retrieved August 6, 2019
- ^ a b Cox TC (March 2004). "Taking it to the max: the genetic and developmental mechanisms coordinating midfacial morphogenesis and dysmorphology". Clinical Genetics. 65 (3): 163–176. doi:10.1111/j.0009-9163.2004.00225.x. PMID 14756664. S2CID 22472334.
- ^ a b Loenarz C, Ge W, Coleman ML, Rose NR, Cooper CD, Klose RJ, et al. (January 2010). "PHF8, a gene associated with cleft lip/palate and mental retardation, encodes for an Nepsilon-dimethyl lysine demethylase". Human Molecular Genetics. 19 (2): 217–222. doi:10.1093/hmg/ddp480. PMC 4673897. PMID 19843542.
- ^ Millicovsky G, Johnston MC (September 1981). "Hyperoxia and hypoxia in pregnancy: simple experimental manipulation alters the incidence of cleft lip and palate in CL/Fr mice". Proceedings of the National Academy of Sciences of the United States of America. 78 (9): 5722–5723. Bibcode:1981PNAS...78.5722M. doi:10.1073/pnas.78.9.5722. PMC 348841. PMID 6946511.
- ^ Shi M, Wehby GL, Murray JC (March 2008). "Review on genetic variants and maternal smoking in the etiology of oral clefts and other birth defects". Birth Defects Research. Part C, Embryo Today. 84 (1): 16–29. doi:10.1002/bdrc.20117. PMC 2570345. PMID 18383123.
- ^ Honein MA, Devine O, Grosse SD, Reefhuis J (November 2014). "Prevention of orofacial clefts caused by smoking: implications of the Surgeon General's report". Birth Defects Research. Part A, Clinical and Molecular Teratology. 100 (11): 822–825. doi:10.1002/bdra.23274. PMC 4559232. PMID 25045059.
- ^ Bell JC, Raynes-Greenow C, Turner RM, Bower C, Nassar N, O'Leary CM (July 2014). "Maternal alcohol consumption during pregnancy and the risk of orofacial clefts in infants: a systematic review and meta-analysis". Paediatric and Perinatal Epidemiology. 28 (4): 322–332. doi:10.1111/ppe.12131. PMID 24800624.
- ^ Hurst JA, Houlston RS, Roberts A, Gould SJ, Tingey WG (October 1995). "Transverse limb deficiency, facial clefting and hypoxic renal damage: an association with treatment of maternal hypertension?". Clinical Dysmorphology. 4 (4): 359–363. doi:10.1097/00019605-199510000-00013. PMID 8574428. S2CID 6330050.
- ^ Boyles AL, Wilcox AJ, Taylor JA, Meyer K, Fredriksen A, Ueland PM, et al. (February 2008). "Folate and one-carbon metabolism gene polymorphisms and their associations with oral facial clefts". American Journal of Medical Genetics. Part A. 146A (4): 440–449. doi:10.1002/ajmg.a.32162. PMC 2366099. PMID 18203168.
- ^ De-Regil LM, Peña-Rosas JP, Fernández-Gaxiola AC, Rayco-Solon P (December 2015). "Effects and safety of periconceptional oral folate supplementation for preventing birth defects". The Cochrane Database of Systematic Reviews. 2015 (12): CD007950. doi:10.1002/14651858.CD007950.pub3. PMC 8783750. PMID 26662928.
- ^ Wehby GL, Goco N, Moretti-Ferreira D, Felix T, Richieri-Costa A, Padovani C, et al. (November 2012). "Oral cleft prevention program (OCPP)". BMC Pediatrics. 12 (1): 184. doi:10.1186/1471-2431-12-184. PMC 3532199. PMID 23181832.
- ^ Costello BJ, Edwards SP, Clemens M (October 2008). "Fetal diagnosis and treatment of craniomaxillofacial anomalies". Journal of Oral and Maxillofacial Surgery. 66 (10): 1985–1995. doi:10.1016/j.joms.2008.01.042. PMID 18848093.
- ^ Tessier P (June 1976). "Anatomical classification facial, cranio-facial and latero-facial clefts". Journal of Maxillofacial Surgery. 4 (2): 69–92. doi:10.1016/S0301-0503(76)80013-6. PMID 820824.
- ^ Allori AC, Mulliken JB, Meara JG, Shusterman S, Marcus JR (March 2017). "Classification of Cleft Lip/Palate: Then and Now". The Cleft Palate-Craniofacial Journal. 54 (2): 175–188. doi:10.1597/14-080. PMID 26339868. S2CID 207236616.
- ^ Sreejith VP, Arun V, Devarajan AP, Gopinath A, Sunil M (2018). "Psychological Effect of Prenatal Diagnosis of Cleft Lip and Palate: A Systematic Review". Contemporary Clinical Dentistry. 9 (2): 304–308. doi:10.4103/ccd.ccd_673_17. PMC 5968700. PMID 29875578.
- ^ Bristow L, Bristow S (2007). Making faces: Logan's cleft lip and palate story. Oakville, Ontaria, CA: Pulsus Group. pp. 1–92.
- ^ a b c d Gill DS, Naini FB (2011). Orthodontics: Principles and Practice. p. 257.
- ^ Lydiatt DD, Yonkers AJ, Schall DG (November 1989). "The management of the cleft lip and palate patient". The Nebraska Medical Journal. 74 (11): 325–8, discussion 328–9. PMID 2586685.
- ^ Sriram Bhat M (2014). SRB's Surgical Operations: Text & Atlas. JP Medical Ltd. p. 414. ISBN 978-93-5025-121-8.
- ^ "Biography and Personal Archive". Archived from the original on June 17, 2007. Retrieved July 1, 2007. at miami.edu
- ^ Barillas I, Dec W, Warren SM, Cutting CB, Grayson BH (March 2009). "Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients". Plastic and Reconstructive Surgery. 123 (3): 1002–1006. doi:10.1097/PRS.0b013e318199f46e. PMID 19319066. S2CID 24514123.
- ^ Maillard S, Retrouvey JM, Ahmed MK, Taub PJ (September 30, 2017). "Correlation between Nasoalveolar Molding and Surgical, Aesthetic, Functional and Socioeconomic Outcomes Following Primary Repair Surgery: a Systematic Review". Journal of Oral & Maxillofacial Research. 8 (3): e2. doi:10.5037/jomr.2017.8302. PMC 5676312. PMID 29142654.
- ^ Fukuyama E, Omura S, Fujita K, Soma K, Torikai K (November 2006). "Excessive rapid palatal expansion with Latham appliance for distal repositioning of protruded premaxilla in bilateral cleft lip and alveolus". The Cleft Palate-Craniofacial Journal. 43 (6): 673–677. doi:10.1597/05-109. PMID 17105324. S2CID 34126577.
- ^ a b Kloukos D, Fudalej P, Sequeira-Byron P, Katsaros C (August 2018). "Maxillary distraction osteogenesis versus orthognathic surgery for cleft lip and palate patients". The Cochrane Database of Systematic Reviews. 8 (8): CD010403. doi:10.1002/14651858.CD010403.pub3. PMC 6513261. PMID 30095853.
- ^ Nasser M, Fedorowicz Z, Newton JT, Nouri M (January 2008). Nasser M (ed.). "Interventions for the management of submucous cleft palate". The Cochrane Database of Systematic Reviews (1): CD006703. doi:10.1002/14651858.CD006703.pub2. PMID 18254111.
- ^ Steele D, Adam GP, Di M, Halladay C, Pan I, Coppersmith N, et al. (2017). Tympanostomy Tubes in Children With Otitis Media. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 28817250.
- ^ Browning GG, Rovers MM, Williamson I, Lous J, Burton MJ (October 2010). "Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children". The Cochrane Database of Systematic Reviews (10): CD001801. doi:10.1002/14651858.CD001801.pub3. PMID 20927726. S2CID 43568574.
- ^ a b Reilly S, Reid J, Skeat J, Cahir P, Mei C, Bunik M (2013). "'ABM clinical protocol #18: guidelines for breastfeeding infants with cleft lip, cleft palate, or cleft lip and palate, revised 2013.', Academy of Breastfeeding Medicine" (PDF).
- ^ Matsunaka E, Ueki S, Makimoto K (October 2015). "Impact of breastfeeding or bottle-feeding on surgical wound dehiscence after cleft lip repair in infants: a systematic review protocol". JBI Database of Systematic Reviews and Implementation Reports. 13 (10): 3–11. doi:10.11124/jbisrir-2015-2336. PMID 26571277. S2CID 45396841.
- ^ Bessell A, Hooper L, Shaw WC, Reilly S, Reid J, Glenny AM (February 2011). "Feeding interventions for growth and development in infants with cleft lip, cleft palate or cleft lip and palate". The Cochrane Database of Systematic Reviews. 2011 (2). John Wiley & Sons, Ltd: CD003315. doi:10.1002/14651858.cd003315. hdl:10072/172084. PMID 21328261.
- ^ a b Duarte GA, Ramos RB, Cardoso MC (September 1, 2016). "Feeding methods for children with cleft lip and/or palate: a systematic review". Brazilian Journal of Otorhinolaryngology. 82 (5): 602–609. doi:10.1016/j.bjorl.2015.10.020. PMC 9444722. PMID 26997574.
- ^ Scalzone A, Flores-Mir C, Carozza D, d'Apuzzo F, Grassia V, Perillo L (February 2019). "Secondary alveolar bone grafting using autologous versus alloplastic material in the treatment of cleft lip and palate patients: systematic review and meta-analysis". Progress in Orthodontics. 20 (1): 6. doi:10.1186/s40510-018-0252-y. PMC 6369233. PMID 30740615.
- ^ Hodgkinson PD, Brown S, Duncan D, Grant C, McNaughton AM, Thomas P (February 2005). "Management of Children with Cleft Lip and Palate: A Review Describing the Application of Multidisciplinary Team Working in This Condition Based Upon the Experiences of a Regional Cleft Lip and Palate Centre in the United Kingdom". Fetal and Maternal Medicine Review. 16 (1): 1–27. CiteSeerX 10.1.1.483.9042. doi:10.1017/S0965539505001452. ISSN 1469-5065. S2CID 36404355.
- ^ "ICHOM | Cleft Lip & Palate Standard Set | Measuring Outcomes".
- ^ Allori AC, Kelley T, Meara JG, Albert A, Bonanthaya K, Chapman K, et al. (September 2017). "A Standard Set of Outcome Measures for the Comprehensive Appraisal of Cleft Care". The Cleft Palate-Craniofacial Journal. 54 (5): 540–554. doi:10.1597/15-292. PMID 27223626. S2CID 43371901.
- ^ "Prevalence of Cleft Lip & Cleft Palate | National Institute of Dental and Craniofacial Research". www.nidcr.nih.gov. Retrieved August 2, 2019.
- ^ See "Who is affected by cleft lip and cleft palate". Archived from the original on March 30, 2008. Retrieved June 20, 2008.
- ^ Cervenka J, Shapiro BL (February 1970). "Cleft uvula in Chippewa Indians: prevalence and genetics". Human Biology. 42 (1): 47–52. PMID 5445084.
- ^ Rivron RP (March 1989). "Bifid uvula: prevalence and association in otitis media with effusion in children admitted for routine otolaryngological operations". The Journal of Laryngology and Otology. 103 (3): 249–252. doi:10.1017/S002221510010862X. PMID 2784825. S2CID 32750501.
- ^ Dobson R (November 2003). "Review of abortion law demanded after abortion for cleft palate". BMJ. 327 (7426): 1250. doi:10.1136/bmj.327.7426.1250-c. PMC 1126893. PMID 14644964.
- ^ Hill, Amelia. "MPs bring bill to ban late abortions for cleft lip, cleft palate and clubfoot," The Guardian, 2020.
- ^ Allison R (December 2, 2003). "Does a cleft palate justify an abortion? Curate wins right to challenge doctors". The Guardian. ISSN 0261-3077. Retrieved September 13, 2024.
- ^ VanderArk S (June 6, 2017). "Edits and Changes to the Text of CS". The Harry Potter Lexicon. Retrieved September 12, 2020.
- ^ Harfield TD. "The Monster Without: Red Dragon, the Cleft-Lip, and the Politics of Recognition" (PDF). Archived from the original (PDF) on February 21, 2014. Retrieved February 5, 2014.
- ^ Plante C (June 14, 2018). "When I asked about Rage 2's worst character, I got an unexpected response". Polygon. Retrieved May 15, 2019.
- ^ Plante C (May 13, 2019). "Rage 2 is a fun game that makes me feel like garbage". Polygon. Retrieved May 15, 2019.
- ^ Nico Van Thyn (June 8, 2012). "Once a Knight: The legendary man, Mr. Byrd". nvanthyn.blogsport.com. Archived from the original on October 5, 2016. Retrieved April 22, 2016.
- ^ Tanner KH (1998). Doc Holliday: A Family Portrait. University of Omaha Press. ISBN 978-0-8061-3036-1.
- ^ "King Tut Not Murdered Violently, CT Scans Show". Archived from the original on July 3, 2007. Retrieved July 1, 2007.
- ^ Bloodfeud: Murder and Revenge in Anglo-Saxon England, Richard Fletcher
- ^ "Tad Lincoln: The Not-so-Famous Son of A Most-Famous President". HistoryBuff.com. Archived from the original on September 27, 2007. Retrieved July 1, 2007.
- ^ "Carmit Bachar, smile ambassador". Archived from the original on October 30, 2007. Retrieved October 13, 2007.
- ^ Beverley Lyons, October 16, 2006. Carmite Doing Her Bit For Charity Archived September 27, 2007, at the Wayback Machine. The Daily Record
- ^ "Jurgen Habermas". Retrieved December 18, 2008.
- ^ "Chat To Ljubo...LIVE". May 28, 2009. Archived from the original on May 31, 2009. Retrieved December 23, 2009.
- ^ "Stacy Keach". Cleft Palate Foundation. Archived from the original on February 13, 2007. Retrieved July 1, 2007.
- ^ "Cheech Marin". Cleft Palate Foundation. Retrieved July 1, 2007.
- ^ Whiteside K (November 4, 2006). "Schmitt is face of West Va. toughness| USA Today". Archived from the original on October 15, 2009. Retrieved April 30, 2010.
- ^ a b "Famous People with a Cleft". April 5, 2008. Archived from the original on January 21, 2013.
- ^ "Who's That Guy? Dario Saric!". September 3, 2014. Archived from the original on August 22, 2014.
- ^ MacEwen A (1910). Antoinette Bourignon, Quietist. London: Hodder and Stoughton. p. 27. Archived from the original on February 6, 2015. Retrieved May 15, 2015.
- ^ Cartwright G (September 30, 2017). "He Was Born With a Cleft Lip". POPSUGAR Celebrity UK. Archived from the original on June 30, 2019. Retrieved May 15, 2019.
- ^ Bartels G (February 18, 2018). "Franz Rogowski im Porträt – Schönheit des Makels". Der Tagesspiegel Online (in German). Retrieved February 6, 2021.
Dass ihm, der Hasenscharte, dem Lispeln und der hellen Stimme wegen auf der Bühne Grenzen gesetzt sind, ist ihm klar.
- ^ a b Ettinger SJ, Feldman EC (1995). Textbook of Veterinary Internal Medicine (4th ed.). W.B. Saunders Company. ISBN 978-0-7216-6795-9.
- ^ Rodriguez Garcia JF (2006). "Surgery of the Soft and Hard Palate". Proceedings of the North American Veterinary Conference. Retrieved April 28, 2007.
- ^ Semevolos SA, Ducharme N (1998). "Surgical Repair of Congenital Cleft Palate in Horses: Eight Cases (1979–1997)" (PDF). Proceedings of the American Association of Equine Practitioners. Archived (PDF) from the original on September 29, 2007. Retrieved April 28, 2007.
- ^ "Mouth". The Merck Veterinary Manual. 2006. Archived from the original on September 29, 2007. Retrieved April 28, 2007.
- ^ Beasley, V. (1999). "Teratogenic Agents". Veterinary Toxicology. Archived from the original on September 20, 2004. Retrieved April 28, 2007.
- ^ Lee JI, Kim YS, Kim MJ, Lee J, Choi JH, Yeom DB, et al. (March 2006). "Application of a temporary palatal prosthesis in a puppy suffering from cleft palate". Journal of Veterinary Science. 7 (1): 93–95. doi:10.4142/jvs.2006.7.1.93. PMC 3242096. PMID 16434860.
- ^ Griffiths LG, Sullivan M (2001). "Bilateral overlapping mucosal single-pedicle flaps for correction of soft palate defects". Journal of the American Animal Hospital Association. 37 (2): 183–186. doi:10.5326/15473317-37-2-183. PMID 11300527.
Further reading
- FIGURE 1 | Development of the lip and palate and FIGURE 2 | Types of cleft in Dixon MJ, Marazita ML, Beaty TH, Murray JC (March 2011). "Cleft lip and palate: understanding genetic and environmental influences". Nature Reviews. Genetics. 12 (3): 167–178. doi:10.1038/nrg2933. PMC 3086810. PMID 21331089.
- Berkowitz S (February 26, 2013). Cleft Lip and Palate: Diagnosis and Management. Springer. ISBN 978-3-642-30770-6.